Behavior and personality often change with dementia. People with dementia often act in ways that are very different from their “old self,” and these changes can be hard for family and friends to deal with. Behavior changes for many reasons. In dementia, it is usually because the person is losing neurons (cells) in parts of the brain. The behavior changes you see often depend on which part of the brain is losing cells.
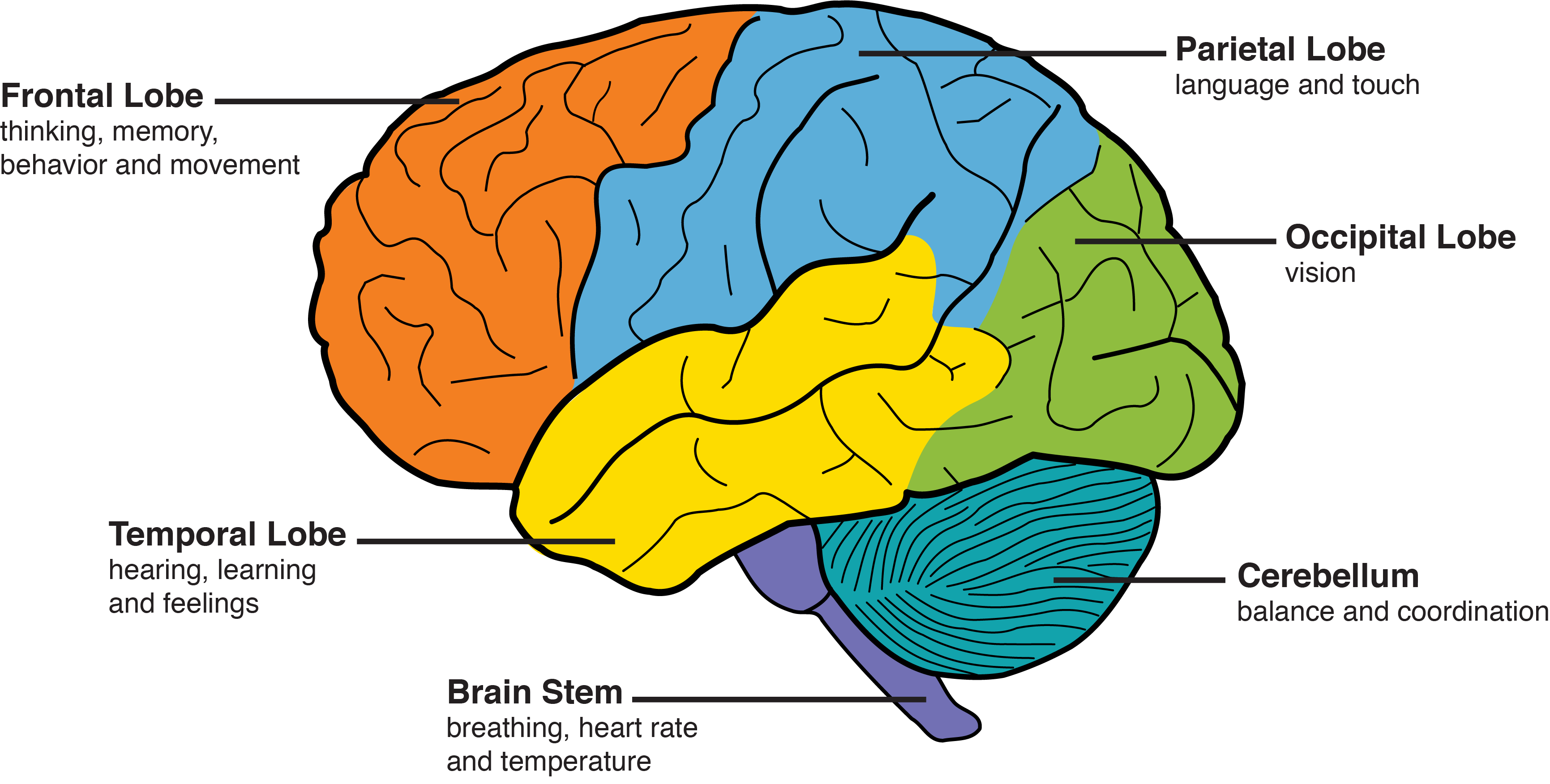
For example, the frontal lobes are the area of the brain right behind the eyes that controls our ability to focus, pay attention, be motivated and other aspects of personality. Therefore, when cells in the frontal lobes of the brain are lost, people are less able to plan and stay focused. They are often less motivated and become more passive. The frontal lobes also control our impulses. Someone with frontal lobe deficits may act rudely or insensitively.
Dementia also alters how a person responds to their environment. A person with Alzheimer’s disease may be forgetful and have trouble following conversations. They may become angry and frustrated because they cannot follow what is going on. Noise, conversation, crowds and activity may be over-stimulating and too difficult to process or understand. Also, many people with dementia rely on others for emotional cues. For example, if you are anxious and worried, many people with dementia will mirror your emotions and become anxious and worried.
Behavior can also change due to medical issues, such as pain or infection. A person with dementia may have a painful condition but may be unable to explain it or describe it. Instead, they may act out in an angry way or be less active. Urinary tract infections, constipation and poor sleep are examples of conditions that can cause sudden changes in the way a person behaves. Finally, some medications may cause changes in the way a person behaves.
What You Can Do
- Consider an evaluation by the person’s health care provider. Sudden changes could be a sign of an infection, pain, or side effect of a medication. Do not assume that behavior and personality changes are always due to dementia.
- While there are medicines that may help soften some behavior changes, medicines are not always the answer. Some behaviors cannot be “fixed” using medicine. For example, no medicine will prevent a person from pacing or wandering. Some medicines can also cause negative side effects and actually make things worse.
- Think of behavior as a form of communication. If the person with dementia acts out in an angry or irritated way, it’s a way of telling others that they may be overwhelmed, in pain, confused or frightened.
- Try to identify what is causing the behavior change. Was there a trigger or something that happened right beforehand? For example, was there an unexpected visitor that disrupted the person’s normal routine? Does the behavior occur at bath time?
- Consider whether the behavior is risky and hazardous, versus annoying and frustrating. Risky and hazardous behavior might be when the person gets angry and tries to walk out of the house in an unsafe manner. You may have to respond in an active way, such as walking with them, distracting them and then installing locks on the door. Annoying and frustrating behavior may require a softer response. For example, if the person paces about the house but is calm and doesn’t try to leave, it may be best to work on accepting that the pacing is okay.
- Try to create a daily routine that is structured and predictable for the person with dementia. Routine is an important source of comfort.
- Foster an attitude of acceptance. The behavioral changes are due to real issues and are not because the person is deliberately trying to be difficult.
- Try to be calm and patient. This means you will need to take breaks. Walk into a different room. Count to 10.
- Talk to other caregivers. Consider a support group where you might learn about helpful strategies that other caregivers have used.
DICE: A Tool for Understanding & Responding to Behavior
D: Describe what Happens
Patient
- What does the patient do?
- How does the patient feel about it?
- Is the patient’s safety at risk?
Caregiver
- How distressing is the behavior?
- Is the behavior threatening your safety?
- Is the behavior causing harm or bringing up bad memories?
- How do you respond to the behavior?
Environment
- Who was there when the behavior occurred?
- When did the behavior occur and how did this relate to other events (e.g., while bathing or at mealtime)?
- Where did the behavior occur?
- What happened before and after the behavior?
I: Investigate Possible Causes
Patient
- Any recent changes in medications?
- Limits in the ability to do things?
- Medical condition (e.g., pain or infection)?
- Unmet need (hungry, tired, bored, lonely, constipated, hearing or vision loss)?
- Underlying mental health issue?
- The severity of cognitive impairment or memory problems?
- Fear, loss of control, embarrassment?
Caregiver
- Could you be misunderstanding the behavior (e.g., thinking the person is “doing this on purpose”)?
- Could you try responding to the behavior differently?
- Are your expectations realistic based on the person’s current abilities?
- Are you dealing with other stressors or mood issues?
- Are there family or cultural issues?
Environment
- Overstimulating environment (noise, clutter, crowds, activities, distractions)
- Boring environment (socially isolated, limited activity)
- Disorienting environment or lack of helpful visual cues?
- Change in routine or lack of a daily routine?
- Activities or tasks do not match current abilities or interests?
C: Create a Plan
Patient
- Respond to possible unmet needs
- Discontinue any high-risk medications
- Follow-up with primary care provider about potential medical causes
- Optimize treatment of mental health issues
- Promote activity during the day and rest at night
Caregiver
- Seek information and support
- Enhance communication
- Create meaningful activities
- Simplify tasks
- Practice self-care
- Get more help (paid or unpaid)
- Talk through worst-case scenario to determine real risks
Environment
- Ensure the environment is safe
- Simplify the environment (reduce clutter)
- Set up the environment for the task at hand
- Enhance the environment (labels, notes, pictures, color contrast or camouflage)
- Create a “command center” for important things (keys, wallet/purse, phone, water, snacks, activities)
- Improve accessibility (grab bars, raised seats)
E: Evaluate the Plan
Patient
- Any new treatments or strategies?
- What worked?
- Have there been any unintended side effects?
Caregiver
- What was tried? Was it helpful or not?
- Are there any barriers to trying something else?
Environment
- What changes have been made? Were the changes helpful or not?
- Are there any barriers to making changes?
Tips for Common Behavior and Mood Changes
Aggressive & Threatening Behavior
Sometimes things can get out of control and feel very scary. These are tips and strategies for dealing with especially challenging behaviors. If you think that you or others may be in immediate danger, call 911.
IF
THEN
The person with dementia is threatening you or acting physically violent, such as hitting, pushing, or kicking you
- Give the person space and time to calm down.
- Stay out of arm’s reach and position yourself near the exit.
- Avoid small spaces like kitchens, bathrooms and cars.
- Remove or secure objects that could be used as weapons.
- Reduce background noise (loud conversations, TV, radio).
- Keep a phone with you in case you need to call for help.
- Go outside, to a neighbor’s house, or public place if needed to stay safe.
- Take a deep breath and try to stay calm.
- Listen.
- Empathize/apologize: “I am sorry this is so frustrating.”
- Offer reassurance: “I know this is difficult. It is going to be okay,” or “I am here to help.”
- Give yourself a break; take time to care for your own needs.
- Get help (medical, emotional, social support, respite).
- Call the Alzheimer’s 24/7 Helpline 1.800.272.3900.
- Call 911 if you think you or others are in imminent danger.
- Tell the dispatcher your name and location and that your family member has dementia. Tell the dispatcher if a weapon is involved.
The person with dementia is angry and accusing you of something that is not true, such as stealing from or cheating on them
- Do not argue or insist that you are right. Avoid using logic and reasoning if the person is insisting on a different reality.
- Avoid confrontational body language, such as crossing your arms and standing over the person or directly in front of them.
- Avoid criticizing, testing, or correcting the person.
- Speak slowly, using a low and soothing pitch.
- Understand how dementia changes the person’s personality and behavior.
- Try not to take the person’s accusations personally.
- Remember that anger or fear responses naturally subside within seconds (in the absence of continued triggers or repeated thoughts).
- People with dementia often forget conflict when the emotional event is not prolonged or repeated.
- Try to make an emotional connection: “I love you. This is hard. We are going to get through this together.
The person with dementia is throwing fits or having emotional outbursts, such as yelling, screaming, or banging on things
- People with dementia often become more sensitive to changes in the environment or routine; try to provide a consistent and predictable routine.
- Simplify the environment; reduce clutter and background noise.
- People with dementia may use your emotions as cues for their own. For example, if you are anxious and worried, they may become anxious and worried. Take a deep breath and try to stay calm and relaxed.
- Ask yourself whether you are expecting too much from the person with dementia. For example, are you expecting them to remember information that they really cannot remember? Adjust your expectations and support the person to function at a level that is most successful for them.
- Consider the emotion the person may be expressing with their behavior. For example, are they afraid of a noise or unfamiliar person? Are they not understanding the conversation and reacting with anger or embarrassment?
- If the person is resistant and uncooperative, stop and try again later with a different approach.
- Provide comforting distractions, such as familiar personal objects or favorite foods and activities.
- Find moments of connection (try using their favorite music, reassuring touch, reminiscing, storytelling, humor, etc.).
Anxiety Related to Dementia
The symptoms of dementia often cause a feeling of insecurity. For example, memory loss may lead to worry about forgetting an appointment while visual-spatial problems can make people feel lost or disoriented even when they are in a familiar place. Having less ability to cope with stress, people with dementia often become dependent on their caregiver to help them manage their emotions. The caregiver may become the person’s “anchor,” or the person they trust who helps them feel secure. The person with dementia might follow or “shadow” the caregiver wherever they go, call the caregiver several times a day on the phone, or ask repeated questions over and over again. They may feel threatened and become agitated when their caregiver feels tired and acts frustrated, or impatient, or when the caregiver tries to ignore them. Similarly, they may become worried and agitated when they cannot find their caregiver, even for a moment. For example, if the person with dementia cannot see or hear their caregiver, they might wander away looking for them and get lost.
This table offers some ideas for helping the person with dementia feel secure. If their anxiety is very distressing or puts their safety at risk, their doctor should be consulted to see if medication might help. Antidepressants are generally safe and can help soften anxiety. Stronger medications like benzodiazepines or antipsychotics have more side effects, although, in some situations, the benefits of the medication outweigh the potential harm.
IF
THEN
The person is following you around and getting worried or agitated when they cannot see or hear you.
- Reduce clutter and background noise that may make the environment disorienting for the person.
- Set up a “control station” near their favorite chair. Make sure they have a snack, some water, an activity or two (e.g., book, puzzle, craft), and any other security objects they prefer (e.g., phone, stuffed animal, purse).
- Consider if the person may need more help or supervision than you are able to provide. Try starting a day program or hiring in-home help. It may take some time but the person will likely adjust to it.
- Reassure the person with a calm tone of voice.
The person is asking the same questions repeatedly or seeking frequent reassurance
- Remind yourself that the person is not doing this on purpose. They have short-term memory loss or a short attention span and they are doing the best they can.
- Use a hearing aid or voice amplifier if hearing loss is an issue.
- Avoid using an annoyed or mocking tone of voice as this is likely to make the person feel defensive.
- Think of a script that you can repeat without having to think about it. For example:
- That was a lovely breakfast (lunch/dinner). Will you help me rinse the dishes?
- It was fun talking with you about that silly cat. I will call you again tomorrow morning. Have a nice time at bingo this afternoon.
- Try to use a matter-of-fact tone of voice. Use humor if you find that the person responds well to it.
- Limit the amount of information you give the person if more information will cause them to worry. For example, you might wait to tell the person about a doctor’s appointment until it is almost time to get ready to go.
- Try to set up a predictable and consistent daily routine for the person. This will help them maintain function and know what to expect.
- If the person lives in a facility, consider setting up a scheduled time to call or visit them each day.
- Keeping a calendar or written daily schedule may be helpful for some people and for others it may cause more confusion.
- Giving the person something to do may distract them from worrying. Often people want to be helpful, try to find simple chores they can help with routinely.
- Regular exercise may be another outlet for nervous energy.
- People with dementia may use your emotions as cues for their own. For example, if you are anxious and worried, they may become anxious and worried. Take a deep breath and try to stay calm.
The person becomes so distressed they are inconsolable
- Take a deep breath and do your best to stay calm yourself.
- Reduce background noise (turn off television) and dim any bright lights if possible.
- Sometimes it helps to have another familiar person, like a neighbor or relative call or visit to distract and reassure the person.
- Arguing with the person or trying to physically restrain them is likely to make the situation worse.
- If there is any immediate threat of danger to the person or anyone else, call 911.
- Contact the person’s doctor to make an urgent appointment to rule out an underlying medical cause and consider pharmacologic treatment.
- If you are at the end of your rope and need help figuring out what to do at any time day or night, call the Alzheimer’s Association’s 24/7 Helpline at 1.800.272.3900.
- If the person responds well to affection, consider holding their hand, giving them a hug, or rubbing their back.
- Consider distracting the person with their favorite food treat like ice cream or chocolate.
- Sometimes people feel calmer when riding in the car or going for a walk. Make sure you bring a cell phone just in case you end up needing to call for help to keep the person safe.
Apathy
Apathy, or indifference, is defined as passivity and a lack of interest or enthusiasm. People with dementia may lose interest in activities or hobbies they once found interesting and fun. They often have trouble coming up with ideas for activities and may rely more on others to come up with things to do. Apathy is one of the most common symptoms of dementia, and the person with dementia is usually not aware of or bothered by it.
Apathy can be hard for families for many reasons. Families may have trouble getting used to passivity in a person who was once motivated and active. Families may worry that the person is sad, because apathy often resembles depression, although not everyone with apathy is depressed. Families may put a lot of effort into finding ways to engage the person with dementia, and this process may be tiring and frustrating. They may feel like they have failed when they are unable to get the person with dementia to be more active. The person with dementia often needs help from others to plan, set up, and start an activity. As the disease progresses, they will need more help to do simpler things. Finally, families may worry that inactivity will lead to other health problems.
The truth is, apathy is hard to treat. There are no medications to treat apathy, although donepezil (Aricept®, used in people with Alzheimer’s disease) can sometimes improve it. In many cases, the area of the brain (the frontal lobes) that makes a person active and interested is affected by dementia. The person with dementia may not be able to start an activity on their own, but they may be able to engage once someone helps them get started. Sometimes, the person with dementia will need help to stay focused on an activity. Sometimes, activities that once held the person’s attention become too much for them or too hard to follow. This does not mean the person “just needs to try harder;” they really cannot be active or show that familiar “spark” of interest and enthusiasm.
Things You Can Do to Help
- Do not assume that old activities and hobbies are familiar and fun for the person with dementia; they may have become too difficult and confusing.
- Work on accepting that apathy is a symptom of dementia and try not to think of the person as being lazy. Find ways to appreciate the person as they are now, with less drive and interest than they had before.
- Do not expect the person with dementia to suggest things to do.
- Try to not let this become an area of conflict between you and the person with dementia. The conflict is not good for either of you!
- Consider simpler physical exercise, such as walking, that is more “automatic.”
- Try simpler activities that the person can do without being frustrated. For example, large piece puzzles, riding in the car, listening to music, and sorting, folding, or stacking objects, are some things that the person may enjoy doing.
- Notice when they are having trouble with a task and offer enough help so that they can be successful without taking over. For example, if the person has difficulty starting a puzzle, you might help by telling them to sort the pieces by color first, then separate the edge pieces, etc.
- Avoid asking open-ended questions that may result in the patient saying “no” or “nothing.” For example, instead of asking, “What do you want to do today?” ask, “What coat do you want to wear for our walk?”
- Set a routine for activities. For example, try playing cards every day after dinner. Knowing what to expect may make it easier for the person with dementia.
- For people who live in a care facility and who do not want to do group activities, ask if the activity director can offer one-on-one activities in the person’s room.
Resource
- The Alzheimer’s Association website has a list of things to do that could be enjoyable for people with dementia
Delirium & Dementia
Is this change in behavior caused by the dementia?
When people notice a change in behavior, like increased confusion or agitation, they often ask whether the change is being caused by the dementia or if it is a sign of something else. This is a good question because it can be hard to tell! While a slow decrease in the person’s abilities over time is expected with most types of dementia, sudden changes that happen over hours or days may be a sign of what is called delirium. It is important to compare new behaviors or changes in abilities to the person’s usual abilities and behavior patterns. With careful assessment, the underlying causes of delirium can often be treated, helping the person recover some or all of their previous abilities.
What are the signs of delirium?
- Changes that occur over hours or days and seem to come and go, or fluctuate throughout the day:
- Change in energy or alertness
- More sleepy than usual, or
- Hyperactive and anxious
- Inability to focus or pay attention; more easily distracted
- Communication problems, such as switching topics too often or using words that do not make sense
- Paranoid thinking or fear that someone or something is trying to harm them
- Seeing or hearing things that are not there
- Movement problems, such as moving slowly, fidgeting, or clumsiness
- Change in energy or alertness
What causes delirium?
Many things can cause delirium, and sometimes there is more than one cause. Here are some common things we look for:
- Infection, such as urinary tract or respiratory
- Medication side effects
- Dehydration
- Constipation
- Urine retention or inability to empty the bladder completely (especially in older men)
- Pain
- Lack of sleep
- Nutritional problems from not eating well
- Electrolyte imbalance (such as low levels of sodium in the person’s blood)
- Other medical problems (diabetes, liver disease, kidney disease, lung disease or heart failure)
What can you do to help?
If you suspect that someone is experiencing delirium, it is important to make an appointment for him or her to see their primary care provider as soon as possible. Their provider may order urine and blood tests to look for possible causes of delirium. It may be helpful for the provider to know what happened before and after the changes in the person’s behavior occurred. If the person seems dramatically different, extremely distressed, or has difficulty breathing, call 911 or take them to a hospital.
Things to help the person get back to “normal” as soon as possible
When someone has delirium, they often feel disoriented, anxious, and frightened. It can be hard for them to feel comfortable or trust that they are safe. Here are some ways to help once treatment has been started:
- Try to stay calm and peaceful yourself
- Reassure the person that everything will be okay
- If the person seems aware that something is wrong, it’s okay to try to talk to them about what is happening. If talking about being sick is distressing for the person, then it’s probably best to avoid talking about it directly
- Promote activity during the day:
- Help the person out of bed for meals
- Take the person on a short walk three times a day (around the house is okay)
- Engage the person in simple calming activities
- Look at picture books or magazines
- Tell stories about the past
- Offer soothing touch (hand, foot, or back rub, brushing hair)
- Help with simple puzzles or adult coloring books, play music or cards
- Demonstrate deep breathing and encourage them to do the same
- Promote sleep at night:
- Minimize light and noise if it disrupts their sleep
- Make sure they are comfortably warm
- Look for any signs of pain (grimace, moan, or bracing with movement)
- Help them stay nourished and hydrated, offer snacks and encourage them to drink throughout the day
- Help them wear any glasses or hearing aids that they normally use
Delirium may begin to improve as soon as underlying causes are treated; however, it can take months for the person to return to their previous level of function and behavior. Unfortunately, delirium can cause dementia to progress more quickly, and in some cases, the person may not be able to fully recover their previous abilities.
Follow-up with the primary care provider
It’s a good idea to schedule a follow-up visit with the person’s primary care provider within a month or so. The provider should check to see if any medications they ordered were helpful. This may also be done over the phone if symptoms have improved. Any medications that were used to help manage psychotic symptoms from delirium may be discontinued (in consultation with the provider) once the person has recovered. If the person has become weak or has more difficulty walking, the provider can make a referral for physical therapy.
For more information:
Delusions & Hallucinations in Dementia
People with dementia sometimes develop delusions or false beliefs, and hallucinations or they sense things that are not actually there. Delusions in dementia may be paranoid; for example, the person might believe someone is stealing from them, their spouse is cheating on them, or someone is out to get them. Delusions in dementia can also be related to memory loss. For example, the person might believe they have to go to work (when they’ve been retired for years), that they are able to drive safely (though their license was revoked) or that they need to take care of their children (who are now grown adults).
Hallucinations involve seeing, hearing, feeling or smelling things that are not there. Hallucinations in dementia may be pleasant; for example, the person might see and talk to “little people,” animals or a person from their past (like a deceased parent). Hallucinations in dementia can also be scary and distressing. For example, the person might hear people yelling at them, see people coming after them or feel bugs crawling on their skin. Strong emotional memories from the person’s past may re-manifest as delusions and hallucinations in dementia. The person may have trouble separating past experiences from current reality and may re-live these events to a certain extent. For example, experiences of abuse, traumatic incidents or tragic loss may be triggered by environmental cues and re-experienced as a delusion or hallucination.
Delusions and hallucinations can occur in all types of dementia and they are especially common in Lewy body dementia (LBD) and Parkinson’s disease dementia (PDD). Things in the environment can contribute to misperceptions. For example, dramatic or scary television programs might be perceived as actually happening in real life. Alarming noises, reflections in a mirror or window, dark shadows and glaring lights can be perceived as someone coming after them. Fatigue or lack of rest can make these symptoms worse. If the symptoms are new or getting worse, it is important to have the person evaluated by their doctor to rule out an underlying medical cause. Sudden changes in mental status can be caused by urinary tract infections, pneumonia, constipation, dehydration and other conditions.
When the person is not bothered or distressed by their hallucinations or delusions, it is generally best to acknowledge their experience with a matter-of-fact tone of voice without endorsing or denying it. For example, you might say something like, “Oh, that’s interesting,” or “Hmm, I don’t see that,” or “Wouldn’t it be nice to have a private jet, they sure cost a lot of money!” and move on to another topic of conversation. Stay calm and avoid arguing with the person or telling them that they are wrong.
This section offers some ideas for helping the person with dementia when they are having delusions or hallucinations. If their symptoms are distressing, their doctor should be consulted to rule out other causes, and see if medication might help. Acetylcholinesterase inhibitors like donepezil (trade name Aricept) or rivastigmine (trade name Exelon) are often helpful. Stronger medications like antipsychotics have more side effects, though the benefits of the medication sometimes outweigh the potential harm.
IF
THEN
The person believes they have to go to work or take care of a previous responsibility
- Remember that the person has a disease that affects their brain and they are not acting this way on purpose.
- Consider ways to adapt former roles. If the person has always been ‟a provider” or ‟a nurturer,” they might help take care of a pet or garden. If they’re used to being in charge, they might be a ‟director” and tell others how to do things they used to do (like cook or fix things).
- Avoid arguing or trying to reason with the person; this will often make the situation worse
- Try distracting the person with conversation. For example, ask them to tell you about their work and gradually guide the conversation to a somewhat related topic. If the person is talking about working in an office, you might change the subject to talking about typewriters or computers.
- Try distracting the person with compliments. For example, tell them how much you like their shirt or jewelry and then ask questions about it. Is it their favorite color? Was it expensive?
- Try redirecting the person with another activity. For example, ask for their help to do something else like rearrange furniture, sort the mail, tinker with a broken appliance, sweep the floor or fold laundry.
- Try reassuring the person by telling them a little lie. For example, you might tell them ‘the office is closed today’ or ‘the kids are at school.’ You will need to immediately redirect them to another topic of conversation or an activity to avoid conflict.
- Find ways to show the person your appreciation. For example, thank them for sharing their story with you, teaching you something you didn’t know, making you laugh, etc.
- Real caregivers share their strategies in this video: Conversations with Caregivers video: Playing Along.
The person sees or hears someone coming to get them
- Remember that the person is not doing this on purpose or pretending to see or hear things. They have an illness that affects their brain and they are doing the best they can.
- Empathize with the person’s feelings and offer reassurance. For example, you might say:
- I’m so sorry, that’s a scary feeling. Let’s take a deep breath. I don’t hear anything. Come with me, let’s make sure everything is okay.
- When I feel scared, I like to spend time with my cat (say a prayer, drink some tea, wrap myself in a blanket, watch a heartwarming movie, etc.) Here’s my cat Charlie, isn’t he sweet?
- I am sorry that was so scary. Let’s turn on all of the lights and eat some ice cream until we feel better.
- Avoid telling the person they should not feel scared.
- Comfort the person with a respectful tone of voice as you would comfort any other adult.
- If the person responds well to affection, offer a hug, hold their hand or rub their back.
- Try to observe the environment from the person’s perspective. Search for visual or auditory cues that might be misperceived by the person. Minimize shadows, noises, and objects that could appear or sound scary or disturbing.
- Are there objects that help the person feel secure like a blanket, a stuffed animal, a religious or spiritual item or a photograph? Consider a robotic stuffed animal.
- If the person lives alone, this kind of paranoia may be a sign that they need more support and supervision. Consider hiring more in-home care or moving the person to a care facility.
- This video from UCLA’s Alzheimer’s and Dementia Care Program demonstrates helpful strategies.
- Remove or secure guns, knives, and other objects that could be used by the person to try to defend themselves from an innocent person they might falsely believe is after them.
The person believes their spouse or caregiver is an imposter. This is also known as Capgras syndrome.
- Remember the delusion is caused by the disease. The person is not acting like this on purpose.
- Try not to take it personally.
- Sometimes it helps to have a familiar person, like a neighbor or relative, call or visit to reassure the person.
- Arguing with the person or trying to convince them they are wrong is likely to make the situation worse.
- This kind of paranoid delusion is especially difficult for loved ones, particularly the person who is believed to be an imposter
- If you are at the end of your rope and need help, call the Alzheimer’s Association’s 24/7 Helpline at 1.800.272.3900
- Consider joining a support group or getting counseling to help you cope.
- The person with dementia may need to spend some time away from the person they believe to be an imposter.
- Consider hiring in-home help, enrolling the person in a day program or moving the person to another relative’s home or a care facility.
- Listen to an interesting podcast from NPR’s Radiolab program about Capgras Syndrome.
The person is accusing someone of stealing from them or hiding their things
- People with dementia are at risk of being victims of fraud and robbery. It is important to investigate these complaints to see if it really is a delusion.
- Often, the person has misplaced their things and they need someone to calmly assist them in finding them.
- Remember the person is not doing this on purpose; try not to take it personally.
- Avoid arguing with the person; it is generally better to just try to help resolve the issue.
- If you are unable to find the item, apologize to the person for their loss. Offer to try to replace it.
- Help the person organize and store their things in places that are intuitive for them. Create visual cues that help the person locate things
- Purchase backups for things that are frequently misplaced like glasses, a wallet, purses and keys.
- If the person lives in a care facility, use iron-on labels to put their name on clothing, shoes and other personal items.
The person becomes severely distressed, aggressive or impulsively tries to ‟escape”
- Take a deep breath and do your best to stay calm
- Reduce background noise (turn off the television or radio) and if possible, dim any bright lights.
- Sometimes it helps to have another familiar person, like a neighbor or relative, call or visit to distract and reassure the person.
- Arguing with the person or trying to physically restrain them is likely to make the situation worse
- If the person will engage in conversation, try calmly talking about concrete things you observe in the environment to help shift their attention to the present moment. For example, you might describe the weather or the immediate surroundings. Encourage use of all of their senses (look, listen, feel, smell).
- Avoid physically restraining the person unless they are in imminent danger or threatening the safety of others
- If there is any immediate threat of danger to the person or anyone else, call 911.
- Contact the person’s doctor to make an urgent appointment to rule out an underlying medical cause and consider pharmacologic treatment.
- If you are at the end of your rope and need help figuring out what to do at any time day or night, call the Alzheimer’s Association’s 24/7 Helpline at 1.800.272.3900.
- Once the situation de-escalates, consider developing a crisis response plan with the person’s care team to manage situations like this in the future. Here is more information about crisis response plans from the National Association for Mental Illness.
- Sometimes repetitive, rhythmic activities can be grounding for people. For example: rocking on a swing or chair, walking, humming, singing, tossing a ball back and forth, playing a hand drum, hitting a punching bag, etc.
Depression & Dementia
People with dementia often suffer from depression, especially in the early to moderate stages of the disease when they have some awareness of losing their abilities. The person may become self-conscious about saying or doing the wrong thing, and avoid friends and family. They may feel sensitive about others being condescending or treating them like children. They may grieve the future they used to imagine and worry about what will happen to them as the dementia progresses. People with dementia often feel guilty about being or becoming a burden on their loved ones. They often struggle with feeling useless and have difficulty finding ways to be helpful. Sometimes the person can feel utterly hopeless and despairing.
People with dementia who suffer from depression are at risk for suicide and should be evaluated by their doctor or mental health professional. Medications are an important part of treatment for depression. In addition, the person will need a lot of support and encouragement to stay active and engaged. Organizations like the Dementia Alliance International and the Alzheimer’s Association offer peer support groups and other services. Individual and couples counseling can also be helpful. Religious or spiritual communities may offer support. This section offers practical ideas for supporting persons with depression and dementia. These tips are not intended to replace proper medical and mental health treatment.
While this section focuses on the person with dementia, it is important to acknowledge that depression is also very common among family caregivers. Seeking treatment and support for your own physical and mental health should be a top priority. Your health and wellbeing have a direct impact on the person you care for.
IF
THEN
The person is giving up activities and isolating themselves from others
- Remember that the person has an illness that affects their brain and they are doing the best they can.
- Make an effort to try new things together. Brainstorm some ideas and write them down on a “bucket list.” For example: try painting, singing karaoke, cooking a new recipe, dancing, taking a day trip, record yourselves telling stories, play hand drums, do a jigsaw puzzle together, Facetime with friends or relatives, etc.
- Try to think of creative ways to turn day-to-day activities into special rituals. For example, bathing can become “spa day,” watching television can be “movie night,” walking can be “endurance training,” eating a meal can be a “date.” Use words and props that help “set the stage.”
- Consider ways to adapt former roles. If the person has always been “a provider” or “a nurturer,” maybe they can help take care of a pet or garden. If they’re used to being in charge, maybe they can be a “director” and tell others how to do things they used to do (like cook or fix things).
- Ask other people to make regular lunch or coffee dates with the person. You can use websites like lotsahelpinghands.com to coordinate your support team.
- Find ways to show the person your love and appreciation.
- Consider more passive activities like going for a drive, listening to music, watching old movies or television shows, observing nature or people from a bench or window.
- If the person is apathetic due to their dementia, it may be best to lower expectations about their level of engagement. Sometimes caregivers have to give themselves permission to stop trying so hard to get the person to do things.
The person appears sad and becomes tearful or cries easily
- Remember that the person is not doing this on purpose or trying to make you feel bad. They have an illness that affects their brain and they are doing the best they can.
- If the person responds well to affection, offer a hug, hold their hand, or rub their back.
- Empathize with the person’s feelings even if why they are sad or crying does not make sense to you. Sometimes the person themselves will not understand or be able to articulate why they feel the way they do.
- Here are some examples of helpful things to say:
- You seem sad to me today. Is there something bothering you? Can we talk about it?
- I am sorry this is so difficult, I want to help. We’ll get through this together.
- Avoid telling the person they should not feel sad.
- Comfort the person as you would comfort any normal adult with a respectful tone of voice.
- Avoid using terms of endearment that are commonly used for children and might be condescending to an adult.
- If the person seems to be stuck in negative thoughts, validate their thoughts/feelings, and then try to gently redirect them to something else. For example, you might say:
- When I feel sad, I like to go for a walk (eat ice cream, hit a punching bag, bake cookies, watch a movie, etc.) Will you join me? Let’s try going for a walk.
- I am sorry things are so hard. I wish there was more we could do about it. For now, maybe we can try to go out and enjoy an ice cream together?
- Consider helping the person join a peer support group. If one is not available in your area, others have found 12-step groups helpful.
- Consider holding a family meeting if there is conflict or misunderstanding among family members that is affecting the person.
- Limit access to alcohol and monitor for overuse.
- Remove or secure guns, medications and other things that could be used for self-harm.
The person becomes severely distressed or inconsolable
- Take a deep breath and do your best to stay calm.
- Reduce background noise (turn off the television) and dim any bright lights if possible.
- Sometimes it helps to have another familiar person, like a neighbor or relative call or visit to distract and reassure the person.
- Arguing with the person or trying to physically restrain them is likely to make the situation worse.
- If there is any immediate threat of danger to the person or anyone else, call 911.
- Contact the person’s doctor to make an urgent appointment to rule out an underlying medical cause and consider pharmacologic treatment.
- If you are at the end of your rope and need help figuring out what to do at any time day or night, call the Alzheimer’s Association’s 24/7 Helpline at 1.800.272.3900.
- Once the situation de-escalates, consider developing a crisis response plan with the person for managing situations like this in the future. Here is more information about crisis response plans from the National Association for Mental Illness.
Impulsive or Disinhibited Behavior
IF
THEN
If the person says or does socially and/or sexually inappropriate things such as:
- Making rude, suggestive, or sexually explicit comments
- Touching themselves or others inappropriately
- Exposing themselves or masturbating in front of others
- Cutting in line, driving aggressively, eating off another person’s plate
- Asking personal or awkward questions, or sharing private information
Remember that the behavior is due to the disease process; changes in the brain can impair the person’s ability to control their impulses or have awareness of other people’s feelings.
Stay calm and try to keep a sense of humor to help soften awkward social encounters. Forewarn family/friends of the person’s behaviors to better prepare them with what to expect and how to best respond to the situation.
Avoid situations that may trigger the behavior, such as crowded or busy public places. Carry "awareness cards" with you as a discrete way to let others know that your companion’s behavior is caused by a brain disorder.
Keep car keys (and sometimes cars) out of sight/reach.
Use distraction; keep the person engaged in other activities to avoid impulsive responses to stimuli in the environment (videos or photos on your smartphone, snacks, objects to fidget with, a magazine or an activity).
Redirect the person to a private space where it they can be naked or masturbate.
Choose clothing that is difficult for the person to remove on their own, but is not restrictive (overalls, clothes with zippers or buttons in the back).
Be consistent with the person about what is okay and what is not okay.
If the person is disruptive or making you or someone else uncomfortable, make eye contact with the person and say, “Stop” with a calm but firm tone of voice, then suggest a different activity such as, “Hold this for me” (putting an object in their hand), “Help me…” (fold laundry, sort magazines, find something), “Let’s get a snack/put on some music/watch TV.”
If you think the person is seeking more physical affection or intimacy, consider pet therapy, a stuffed animal and socially appropriate touching like hand holding, dancing, back rubs or massages, manicure/pedicures or brushing/combing hair.
Talk with the person’s medical provider about any safety concerns related to the behavior. They may be able to report the person to the DMV, write a letter, prescribe medication or give you more ideas for reducing safety risks.
Perseverative or Compulsive Behavior
IF
THEN
If the person repeats a specific task or activity such as:
- Checking locks, doors, window coverings over and over
- Having rigid walking patterns, including pacing
- Collecting or hoarding items
- Counting or organizing objects repeatedly
- Going to the toilet frequently
- Selective eating habits
Remember that this behavior is due to the disease process; the person is not doing this to purposely annoy you and may not have any control over it.
Consider if the behavior is really a problem; if it does not cause any safety risks you might avoid conflict by learning to accommodate it.
Consider if the person might have a need that they are not able to express, such as boredom, hunger, insecurity or needing to use the toilet.
Sometimes people engage in repetitive behavior because they feel anxious, and the repetitive activity is soothing. Consider other ways to help address anxiety.
See if there is a way to substitute the behavior with other activities such as exercise, helping with simple tasks (folding laundry, sweeping, wiping down countertops) or creative projects (drawing, stringing beads, making a collage).
Remove or hide objects in the environment that might trigger the behavior. For example, hide ladders and tools in a secure location.
If the person is very rigid and resistant to any interference with their activity, be careful to avoid an aggressive reaction:
- Use a calm, matter-of-fact tone of voice. Try not to sound bossy or condescending.
- Try to distract the person with something appealing to them like a snack, music, or other favorite activity.
Sleep Disruptions
People with dementia often have problems sleeping and experience changes in their sleep patterns. Some of these changes are part of normal aging. Many of the changes in sleep patterns are caused by the impact of dementia on areas of the brain that control sleep. Many people with dementia sleep more during the day and thus, can be more awake and active at night. They may also awaken more easily during the night. Some people have trouble telling the difference between night and day. These sleep problems often disrupt the caregiver’s sleep. Many caregivers also report that they sleep poorly because they are worried and anxious. Sleep disruption can be stressful and burdensome for family caregivers, and we encourage caregivers to reach out for help.
There are medical conditions that can affect sleep. Depression and anxiety can cause early morning awakening, trouble getting back to sleep and poor sleep quality. Restless legs syndrome is a disorder that causes unpleasant sensations in the legs causing the urge to move. Sleep apnea is a pattern of breathing that results in poor sleep quality. Acting out during sleep (for example, moving, hitting out, and vivid dreams) can disrupt normal sleep patterns. Illnesses, such as angina and congestive heart failure can affect one’s sleep patterns. Anyone experiencing these symptoms should consult their healthcare provider.
Figuring out the Cause(s)
It is important to try and figure out what may be causing the sleep problem. There may be multiple factors: the environment, the daily schedule, having a pet, the result of dementia, and/or the types of medications being taken. Figuring out the cause is an important step in deciding how to manage or treat the sleep disturbance.
Sometimes it is helpful to keep a log or diary to see if there is a pattern to the sleep problem(s). For example, one caregiver slept in her mother’s room and discovered there was a bright light coming from a street lamp and that the neighbor routinely started their noisy car early in the morning. Moving her mother to a quieter, darker bedroom helped them both get better sleep.
If you have insomnia, you may experience one or a combination of the following symptoms:
- Taking a long time (more than 30 to 45 minutes) to fall asleep
- Waking up several times each night
- Waking up early and being unable to get back to sleep
- Waking up feeling tired and not able to function well during the day
Managing & Treating Sleep Problems
There are drug and non-drug approaches to the treatment of sleep disruption. Most experts encourage the use of non-drug strategies. Sleep medications are associated with a greater chance of falls and other risk factors. The following are strategies that can be used for the person with dementia and the family caregiver.
Set the Right Environment
- Keep a regular schedule: go to bed and get up at the same time every day.
- Try to exercise daily but not within three hours of bedtime.
- Make sure the temperature in the bedroom is comfortable (not too hot and not too cold).
- Reduce liquid intake before bedtime.
- Try not to nap during the day; if you do nap, try to do so before 3 p.m. and try to keep the nap short (about 20 minutes).
- Keep the bedroom as dark and quiet as possible; use a nightlight if needed, but be aware that bright light disrupts sleep/wake patterns.
- Calm activities at the end of the day and before bedtime may help with sleep.
- Avoid violent movies or TV shows; strong content and images can be upsetting and can make it hard to relax.
- Be aware that changes in your environment, such as moving to a new home or having unexpected visitors can be disruptive and confusing for the person with dementia.
- Avoid alcohol and products that contain caffeine (tea, chocolate or soda) and nicotine; these can cause overstimulation and interfere with sleep.
- Have access to daylight for several hours a day; exposure to light improves day/night patterns.
- For the person with dementia, avoid keeping their daytime clothing in view at night; this may be a cue that it’s time to get up.
Medications for Sleep
- Always talk with your healthcare provider before using over-the-counter (OTC) sleep medicines; many of them can make confusion worse, and some common OTC medications (like Tylenol PM) contain Benadryl, which can actually worsen sleep and cause confusion in older adults.
- Ask your health care provider if any of the medication you currently take could be causing sleep disruption.
- If the person with dementia is taking a cholinesterase inhibitor (donepezil, rivastigmine or galantamine), avoid giving the medicine before bed; instead, give it in the morning.
- Be aware that medicines used to promote sleep carry risks for older adults and people with dementia, including imbalance and falls, fractures, and increased confusion.
- Consider whether using a sleeping medication is appropriate; selective serotonin reuptake inhibitors (SSRIs) are a commonly used type of medicine (i.e., trazodone).
- Any time you are prescribed a new medication, make sure to ask your healthcare provider about possible benefits and risks; ask about other treatment options that may be available.
Other Things to Consider
- Be sure to treat conditions that may be causing pain and discomfort; consider using an analgesic at bedtime if your health care provider agrees.
- Do not restrain a person with dementia to keep them in bed; this can create agitation and a desire to escape and can lead to a fall or injury.
- Consider installing security alarms on doors and windows if there is concern that the person with dementia might wander from the house during the night; knowing that you have an alarm system may help you get better sleep.
- Consider using a bedside commode if getting up to the bathroom is causing sleep disruption.
- If you think being hungry at night is a problem, have a light snack just before bed.
- Use the toilet right before bedtime to help prevent nighttime waking.
- Consider hiring help in the home during the nighttime hours to help you, as the caregiver, get some sleep.
- There is evidence that meditation and mindfulness promote good sleep.
Other Resources
- 6 Tips for Managing Sleep Problems in Alzheimer’s (NIA)
- A Good Night’s Sleep (NIA)
- Dementia and Sleep (Sleep Health Foundation)
- Good Sleep Habits (Sleep Health Foundation)
Wandering & the Risk of Getting Lost
Any person that has memory problems and is able to walk is at risk for wandering and getting lost. Wandering can happen at any time. Wandering may be triggered by an attraction to something in the environment such as a shiny doorknob or elevator buttons. Persons with dementia may also be responding to an impulse or need to “go somewhere” or “do something.” Sometimes a person may get lost because they are, or become, disoriented. Some people wander because they are confused or frightened. Wandering is not necessarily a problem unless the person is at risk for getting injured, being taken advantage of, or getting lost.
IF
THEN
Your loved one with dementia can get around by themselves
Prepare for the possibility that they may wander and get lost:
- Keep a recent, close-up photograph or video of the person in an accessible place, such as your wallet or cell phone.
- Inform family, friends, paid caregivers, and neighbors that the person is at risk for wandering and getting lost; ask that they keep an eye out for the person and alert you if they see them out and about on their own.
- Inform local public servants and business owners, such as the police, fire department and store clerks, that the person is at risk for wandering and getting lost and make sure they have your phone number
- Make a list of likely places where the person may wander in case you need to search for them (past jobs, former homes, places of worship or favorite restaurants)
- Consider using an alarm, chime, or bell to alert you when the person is exiting a room or leaving home unattended
- Try to provide enough supervision to keep the person safe; consider hiring an in-home caregiver or companion or enrolling the person in a day program
- Try to keep the person engaged in a familiar routine each day, since unexpected changes and over- or under-stimulation can be a trigger for wandering
- Consider enrolling the person in the MedicAlert®+Alzheimer’s Association Safe Return® program at 1.800.625.3780
- Consider getting the person an ID bracelet or necklace with your contact information on it
- Consider using a GPS tracking device or smartphone application that uses satellite technology to locate missing persons carrying or wearing a sensor device (i.e., shoe insert, watch or anklet)
Your loved one is actively trying to leave, for example, to “go home” even though they are at home or “Go to work” even though they no longer work
Environmental Strategies:
- Hide environmental “exit cues” or “trigger items,” such as keys, shoes, jackets, hats and purses.
- Simplify the environment; reduce clutter, crowding, and background noise. Some television programs can be distressing.
- Try placing a large “DO NOT ENTER” sign on exit doors.
- Camouflage exit doors by painting them the same color as the walls or covering them with a removable curtain or screen.
- Cover knobs with cloth the same color as the door or use childproof knobs.
- Do not lock a person with dementia in the home or in a car unattended.
- Do not try to physically restrain a person with dementia unless you are attempting to protect them or others from immediate harm (such as getting hit by oncoming traffic).
Communication Strategies:
- Avoid trying to convince the person that they are already home or that they no longer work. This will lead to an argument and make the person more insistent about what they believe to be true.
- Try to go along with what the person is saying and guide them to something else without letting them realize they are being redirected.
- Remember to be calm and reassuring instead of controlling.
- Try making an emotional connection with the person in that moment.
- Use communication that is supportive and focused on distraction, for example:
- “What was it like growing up in your house?”
- “What is your favorite room in the house?”
- “We can leave after lunch. Can you help me set the table?”
- “I love you. This is hard. We are going to get through this together.”
The person tries to leave because they are frightened and agitated
- Stay calm. Consider calling a neighbor or friend to be on standby in case you need help.
- Avoid running after them or trying to hold them back unless there are obvious hazards, such as traffic or harsh weather. Chasing after them may make the situation more dangerous.
- Follow the person from a distance to give them personal space. Try to redirect their train of thought in a gentle manner. Some people will respond to verbal redirection, such as pointing out the weather or some other observation of the present moment:
- “It sure is gray and cold out today. Would you join me for some hot cocoa?”
- “Look at those cherry blossoms – how lovely! What is your favorite flower?”
- Use positive directions rather than negative. For example, say, “Come with me,” not “Stop, don’t go there.”
- Notice what may have triggered this behavior, for instance, a loud noise, a crowded or busy space, a change in routine, or your own emotional state.
Your loved one seems bored or restless
- Encourage exercise to help reduce anxiety, agitation, and restlessness. Go for a walk, rock in a bench swing, toss a beach ball, dance or participate in group exercises.
- Find moments of connection (try using their favorite music, reassuring touch, reminiscing, storytelling, humor, pets, gardening or conversation).
- Try going outside to experience a change in scenery (get a snack or an ice cream cone, visit a pet store, museum or mall or take a scenic drive).
If your loved one is missing and you cannot find them
- Call 911 and let them know that a “vulnerable adult” with dementia is missing.
- If you are enrolled, call MedicAlert®+Alzheimer’s Association Safe Return® program at 1.800.625.3780.
- Write down what the person was wearing.
- Call someone to help you (family, friend or neighbor) walk or drive around the block or the immediate area. If possible, have somebody stay at home so that they can answer the telephone and be there in case the person returns.
- Have the person’s most recent photo and medical information ready for police.
- Gather your list of places that the person may wander – past jobs, former homes, places of worship, restaurants, or bars.
- Check dangerous areas near the home, such as bodies of water, open stairwells, dense foliage, tunnels, bus stops and roads with heavy traffic.
Resources
Technology
There is a lot of interest and hope that technology will provide safeguards against the risk of wandering and getting lost. Most products and services have not been studied to see if they are effective. We try to stay up-to-date on what is available but cannot endorse any of the devices or services below.
Smart Phone Applications
- Find My iPhone is a free feature for iPhones
- Life360 is a free application for patients who always carry a smartphone. It uses GPS technology and communicates with other smartphones.
Motion Sensors & Voice Reminders
Tracking Devices
- GPS Smartsole: $300/device, $35/activation, $30/monthly monitoring fee
- S911 Lola Personal GPS Tracker: $185/device and monthly service fee from $50–200/mo, includes extra features like a panic alert button, in/out of fence alert, shock alert, etc. Up to 30 hours battery life.
- Trackimo: $139.99 with first 12-month subscription included, $5/mo after that. A compact GPS tracking device that enables you to track anything from anywhere using your smartphone or computer. Six days of battery life (standby mode)