- Study Director: Joel Kramer, PsyD
- Sponsors: National Institutes of Health and Hillblom Brain Aging Center
- Official Study Title: Brain Aging Network for Cognitive Health
- Conditions Studied: Healthy aging
Purpose of the Study
This is a longitudinal study looking at the effects of aging on cognition in older adults. The purpose of the study is to
- gain a better understanding of the variety of processes that contribute to resilience and resistance in healthy aging, and
- identify the earliest changes associated with degenerative brain disease.
This study also refers healthy volunteers to other Memory and Aging Center projects they may be eligible for. For more information, please visit our Brain Aging Network for Cognitive Health website.
Study Details
Inclusion criteria: Aged 30+ with minor or no memory problems
Exclusion criteria: Significant memory problems or diagnosis of a neurodegenerative disease or other major health condition
What to Expect
Testing: A neurological examination, cognitive testing, fasting blood draw for genetic studies, interview with a study partner (someone who knows you well and can comment on any changes over time in your memory, thinking, personality, or behavior) and follow-up appointments every 12 months.
- Lumbar Puncture: Lumbar punctures are vital to our research efforts at the Memory and Aging Center. CSF collected through lumbar punctures is a primary source to measure markers from the brain in living humans. We now have reliable CSF markers for early detection of Alzheimer’s disease processes for use in the clinic, and many more markers in exploratory stages to help us better understand how the brain ages and how neurodegenerative disease unfolds in humans. If you are interested in participating in an optional lumbar puncture as part of our research study, please read the FAQ below:
Lumbar Puncture FAQ
What is a lumbar puncture (LP)?
Lumbar puncture is a procedure used in clinic and research in which a small amount of fluid is removed by inserting a needle in the lower back, far below where the spinal cord ends. This fluid, cerebral spinal fluid (CSF), bathes the brain and spinal cord.
Why is a lumbar puncture so important?
Lumbar punctures are essential to our research! The cerebral spinal fluid (CSF) we collect is a rich source of proteins and other molecules found in and around the brain. CSF directly reflects the status of the brain and central nervous system.
The brain is protected from the rest of the body by a barrier called the “blood-brain barrier.” Due to this barrier, we cannot capture molecules that are found in CSF directly from the blood. CSF contains some of the earliest markers of abnormal brain changes.
Research from our team and many others have found that changes in CSF predict future risk for cognitive decline and dementia. What we learn has been and continues to be used to develop diagnostic tools and preventative treatments for Alzheimer’s and other neurodegenerative diseases. We need more participants like you to advance these efforts!
What have we learned from lumbar punctures and CSF?
Graph illustrating that only adults with low synaptic functioning showed a relationship between amyloid, tau and neurodegeneration. Thanks to many of your LPs and generous CSF donations, there have been rapid advances in CSF biological markers. We now have reliable markers for early detection of Alzheimer’s disease processes for use in the clinic. These markers are leading to more precise clinical trials. We have many more markers in exploratory stages that are teaching us invaluable information about how the brain ages and how other neurodegenerative diseases unfold in humans. One recent finding from your group CSF data suggested that synaptic integrity (the presence of communication junctions between brain cells) may play a critical role in how the amyloid plaques and tau tangles of Alzheimer’s disease develop.
In a recent study of healthy adults in the Hillblom Aging cohort, we measured CSF levels for two major proteins in Alzheimer’s disease: amyloid “plaques” and tau “tangles.” In Alzheimer’s disease, amyloid is thought to lead to tau, which causes neurodegeneration (breakdown of brain cells). We also measured markers of synapse functioning in CSF. Synapses are the communication junctions between brain cells that transmit signals from one cell to another, and they allow the brain to function. We found that only adults with low synapse markers showed a relationship between amyloid, tau and neurodegeneration.
Adults with high synapse markers did not show the adverse relationship between amyloid and tau. These data suggest that maintenance of synaptic functioning may play an important role in how Alzheimer’s disease markers develop. This study is leading to future projects on how to target synaptic functioning in order to prevent dementia.
Can my lumbar puncture results be shared with me?
At this time, we are still learning more about what CSF biomarkers can predict at a group level. We don’t have enough information to discuss most of the lumbar puncture results on the individual level. With these collective CSF samples, we are trying to tackle neurodegeneration at the earliest stage of change, instead of waiting for symptoms to emerge.
Who performs the lumbar puncture?
Lumbar punctures are performed by board-certified neurologists, who are highly experienced in carrying out this procedure. Many patients at the Memory and Aging Center have received an LP for diagnostic reasons or as part of research visits. Our neurologists are exceptionally trained to guide you throughout the procedure and answer any questions you may have.
What happens during a lumbar puncture?
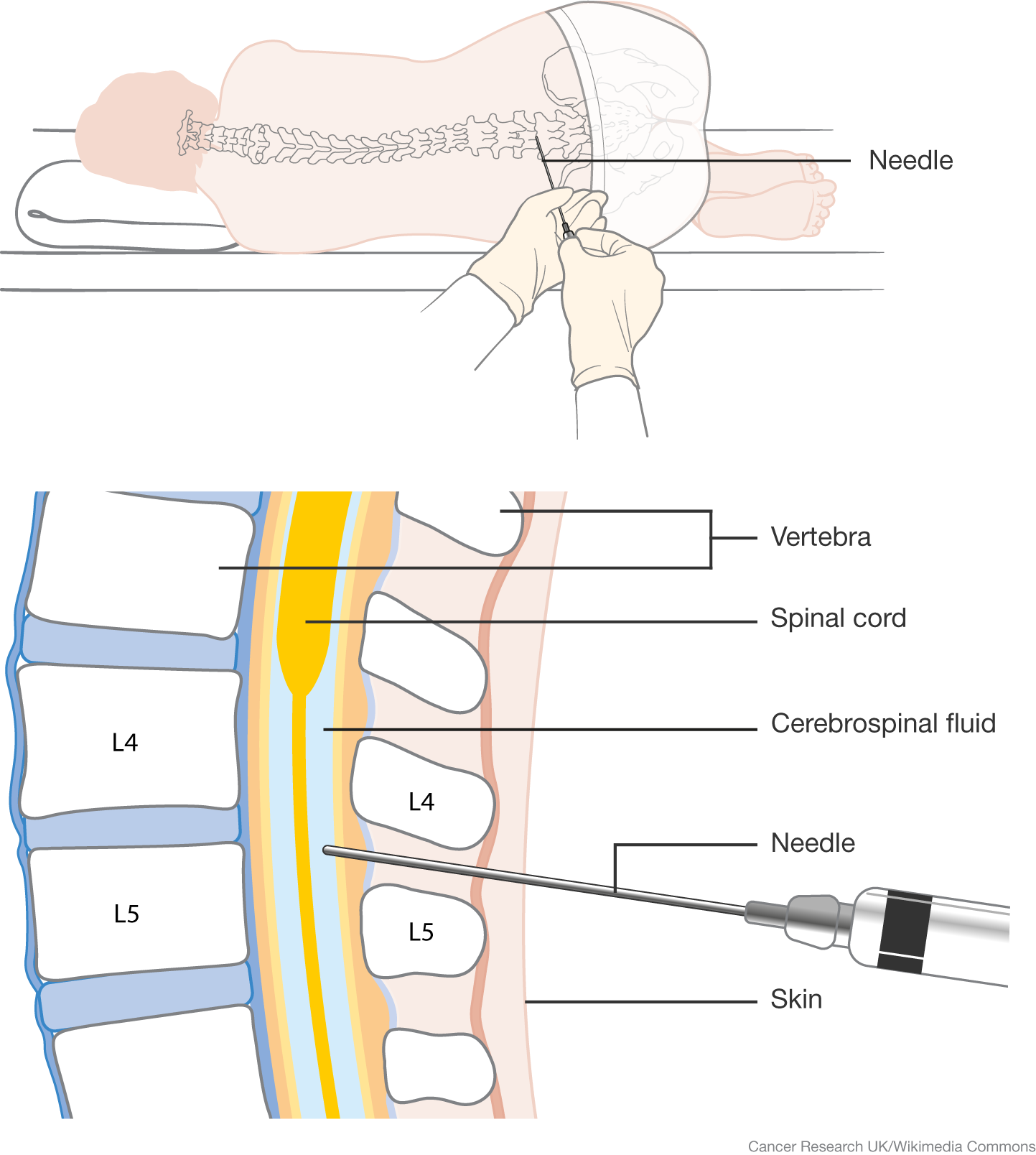
Lumbar puncture procedure. Illustration by Cancer Research UK - Wikimedia Commons Before scheduling a lumbar puncture, we make sure it is a good fit for you. We first take a few extra samples of blood during one of your research blood draws with our center. This process checks for criteria such as clotting factors and platelet counts, and your results are cleared for safety by our neurologists.
During the procedure, you will be accompanied by one of our research coordinators, who is there to support you and provide additional assistance to the neurologist. During the lumbar puncture, you can either lie down on your side or sit upright. The neurologist will feel and massage your back to identify the correct place to insert the needle. This area is between two bones of the lower back (vertebrae L4 and L5), far below the spinal cord. Spinal cord nerves will not be disturbed or at risk of damage during the procedure.
Before inserting the needle, the neurologist will carefully sanitize your back and inject a local anesthetic (Lidocaine). This might feel like a numbing shot at the dentist, but the sensation is less noticeable since the lower back has fewer nerve endings. After the anesthetic kicks in, the neurologist will insert the collection needle. About 2 tablespoons of CSF will be allowed to naturally drip out. You may feel mild contact pressure at the insertion site, but you should not feel any sharp pain.
The procedure takes about 30 minutes. Once the lumbar puncture is complete, you will rest for about 1 hour. We will provide you with a snack and keep you company. Afterward, you should be able to drive home and go about your normal activities, though we advise avoiding strenuous physical activity for the next 24–48 hours.
What happens if I change my mind?
Your participation in research is always voluntary. You can change your mind about an LP any time leading up to the procedure!
What are the risks associated with a lumbar puncture?
The risk of infection from a lumbar puncture is very low, even less than from a standard blood draw. The LP is done in an extremely sterile state with a sterilized kit, sterilized gloves and an antiseptic solution.
The most common side effect after the procedure is a minor headache within the first 24 hours. These headaches are usually position-dependent, so they tend to occur when you are sitting or standing upright. They typically don’t persist for more than a few days and go away when you are lying flat. To reduce your chance of getting headaches after a lumbar puncture, we use a very thin, specialized type of needle. Staying well-hydrated, laying down, drinking caffeinated beverages and taking over-the-counter pain medication are easy ways to relieve any headaches. If the headache persists or worsens, another option we offer is administering a “blood patch,” which works to clot and heal the lumbar puncture site faster.
Common lumbar puncture side effects include:
During Procedure:
- Headache (17.1%)
- Nerve pressure/tingling (14.2%)
- Pain (8.6%) Nausea/dizziness (7.0%)
Post-Procedure:
- Headache (5.5% total; mild 3.7%; moderate 1.4%; severe 0.4%)
- Low back pain (8.5% total; mild 6.7%; moderate 1.8%; severe 0%)
Source: Wisconsin ADRC Lumbar Puncture participants (2021)
Will I be compensated for participating in a lumbar puncture?
We do realize this procedure is more invasive than some of our other procedures and can take a lot of consideration before participating. If you are enthusiastic and willing to complete a lumbar puncture with us, we compensate participants with $100 for donating this time and CSF to our research.
How can I learn more or schedule a lumbar puncture in the future?
If you have any questions or would like to schedule a lumbar puncture, please contact research coordinator Shannon Lee at 415.476.3788 or [email protected].
The Frequency of Visits: One visit (3–5 hours total) every 12 months longitudinally. An additional 2–3 visits (8–12 hours total) are common for participation in subprojects associated with the Brain Aging Program. These additional studies include MRI imaging, PET imaging, sleep actigraphy monitoring, and physical activity studies.
Materials Needed Prior to Evaluation: None
Costs: No costs will be charged for any of the study procedures. Parking will be validated for the 1625 Owens Street Garage or 1630 Third Street Garage at the UCSF Mission Bay campus for all study visits.
Reimbursement: There is no monetary compensation for participation. Your participation is entirely voluntary and is a donation of your time and energy dedicated to improving our understanding of the multitude of factors that impact the aging brain.
Join Our Study
If you are interested in joining the Brain Aging Network for Cognitive Health, please complete this online screen. After filling out the online screen, you may be contacted by the study coordinator, Valentina Diaz to discuss your eligibility. If you have any questions, please contact the study coordinator, Valentina Diaz, at [email protected] or 415.476.1820.
Additional Healthy Aging Program Studies
- Aging and Cognitive Decline: a longitudinal study to identify the cognitive mechanisms and neural structures leading to a decline in executive functioning in both healthy aging and populations affected by mild cognitive impairment
- Vascular Contributions to Cognitive Impairment and Dementia (VCID): a multisite consortium study whose mission is to study the interaction between cerebrovascular disease and neurodegenerative diseases and to develop biomarkers for use in clinical trials
- PET Imaging in Aging Population: a study of protein aggregation in the brain as it relates to brain structure and function in healthy aging
Brain Aging Network for Cognitive Health Symposium
The annual Brain Aging Network for Cognitive Health (BRANCH) Symposium is designed to bring together leading researchers in brain aging to share the latest advances in the field. This full-day event highlights the most recent findings between collaborators of the UCSF Network for the Prevention of Age-Associated Cognitive Decline as well as special guest lectures from experts in the field of cognitive aging. The talks and Q&A panels at the symposium cover a wide range of topics designed to reflect upon prior knowledge and forge future relationships. This event usually occurs in the fall and is open to the public.
Resource Sharing
To request clinical data, external and internal investigators must fill out the Data Request Form.

